Author: Denis Avetisyan
A new study details a collaborative approach to building robots for complex healthcare environments, prioritizing the needs of both patients and practitioners.
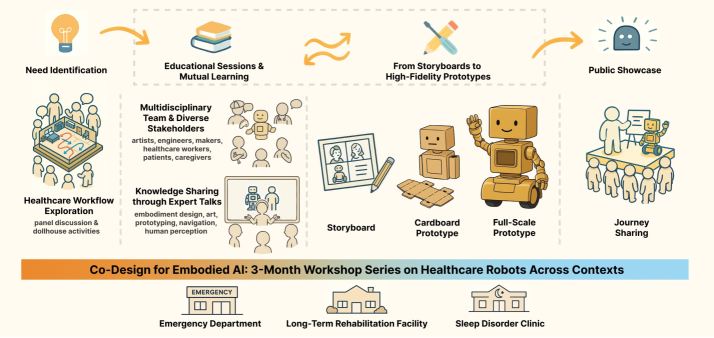
Researchers present a 14-week co-design workshop resulting in high-fidelity prototypes for emergency, rehabilitation, and sleep disorder care settings.
Despite growing interest in embodied artificial intelligence, translating abstract concepts into deployable robotic systems within complex real-world settings remains a significant challenge. This research, ‘Towards Considerate Embodied AI: Co-Designing Situated Multi-Site Healthcare Robots from Abstract Concepts to High-Fidelity Prototypes’, details a 14-week co-design workshop involving healthcare professionals and engineers to develop robot solutions tailored to emergency departments, rehabilitation facilities, and sleep disorder clinics. Findings reveal that iterative prototyping, supported by educational scaffolding, enables participants to navigate real-world trade-offs and generate more viable designs, culminating in eight guidelines for considerate embodied AI. How might these co-design principles be extended to foster more effective and ethically-aligned AI systems across other high-stakes domains?
The Imperative of Human-Centered Design in Healthcare Robotics
Contemporary healthcare systems face escalating pressures from aging populations and increasing complexity of care, often revealing a rigidity in established workflows. These traditionally structured processes frequently struggle to accommodate unexpected surges in patient volume or adapt to the individualized needs of each person receiving treatment. This inflexibility doesn’t merely create logistical bottlenecks; it directly contributes to inefficiencies, potentially leading to delayed interventions, increased risk of medical errors, and elevated stress levels for healthcare professionals. Consequently, a critical re-evaluation of these established protocols is essential, emphasizing the development of more responsive and resilient systems capable of navigating the dynamic demands of modern healthcare delivery.
Successfully incorporating robotic technologies into healthcare hinges not simply on technical feasibility, but on a comprehensive grasp of the needs and expectations of everyone involved – clinicians, patients, and support staff. A human-centered design approach prioritizes understanding these often-complex requirements through direct observation and iterative feedback, ensuring solutions address real-world challenges and seamlessly integrate into existing workflows. This methodology moves beyond simply automating tasks; it focuses on augmenting human capabilities, reducing cognitive load, and improving the overall quality of care. Consequently, robotic systems designed with a deep understanding of stakeholder needs are more likely to be accepted, adopted, and ultimately, to deliver meaningful improvements in healthcare outcomes.
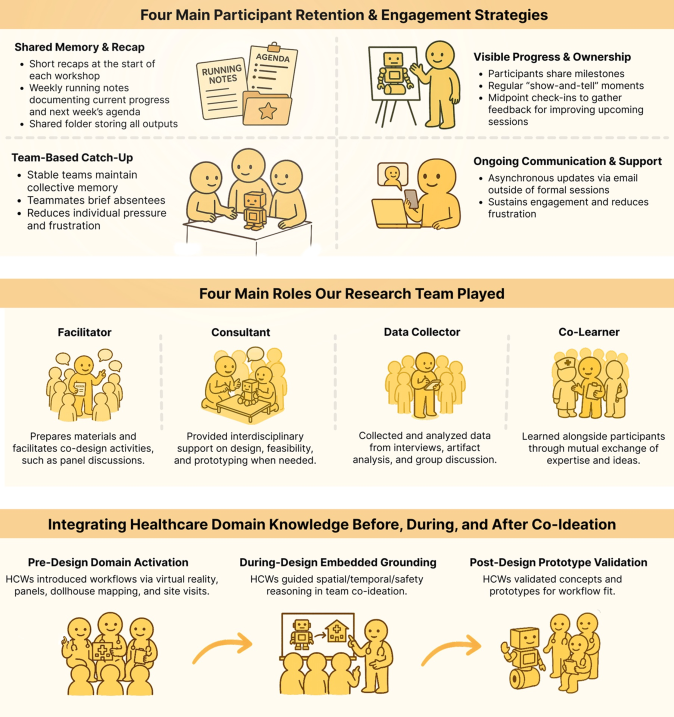
Successful implementation of healthcare robotics hinges on a collaborative design process that actively incorporates the perspectives of clinicians, patients, and technicians. Recent research highlights the effectiveness of co-design workshops in bridging the gap between technological innovation and practical healthcare needs; these sessions successfully integrated diverse stakeholder input to generate detailed robot prototypes and, crucially, actionable guidelines for future development. This approach ensures that robotic systems are not merely technologically advanced, but also seamlessly integrate into existing workflows and genuinely enhance the quality of patient care, rather than introducing new complications or disrupting established practices. The resulting designs prioritize usability, safety, and patient comfort, fostering acceptance and maximizing the potential benefits of robotic assistance in healthcare settings.
Contextual Adaptation: Tailoring Robotic Functionality to Diverse Healthcare Environments
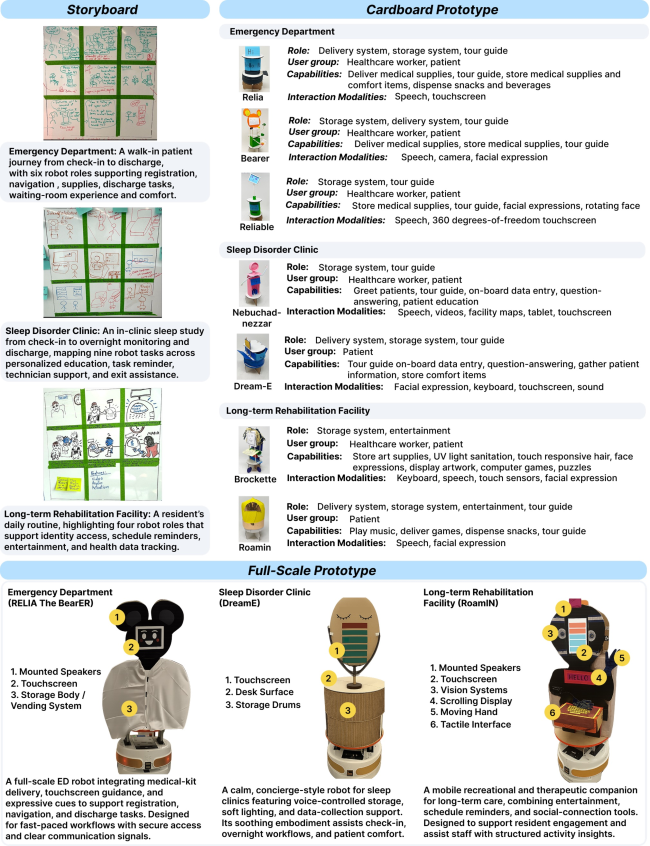
The deployment of robotic systems within healthcare is not uniform, as differing environments necessitate tailored designs and functionalities. Acute care settings, such as emergency departments, present challenges related to rapid response times, logistical complexity, and high patient turnover, requiring robots focused on efficiency and supply chain management. Conversely, long-term rehabilitation facilities emphasize sustained patient interaction and assistance with activities of daily living, demanding robots prioritizing safety, adaptability, and user-friendliness. Specialized clinics, like those addressing sleep disorders, introduce unique data acquisition and therapeutic support needs, driving the development of robots with specific sensor suites and intervention capabilities. These diverse operational contexts mandate a segmented approach to robotic design, acknowledging that a single ‘one-size-fits-all’ solution is impractical given the varied requirements and limitations of each healthcare environment.
Emergency Department (ED) robot designs are centered on improving operational efficiency within high-throughput environments. These robots are engineered to automate front-end processes, specifically patient registration and initial data collection, reducing wait times and administrative burdens on staff. Beyond registration, ED robots facilitate the rapid delivery of essential supplies – medications, lab kits, and medical equipment – to points of care, minimizing delays in treatment. Design considerations prioritize navigation within crowded and dynamic spaces, integration with existing hospital information systems for real-time data access, and adherence to strict hygiene protocols to prevent cross-contamination. The goal is to free up medical personnel to focus on direct patient care by streamlining logistical tasks and optimizing resource allocation.
Long-term rehabilitation facility robot design centers on maximizing patient autonomy and well-being. These robotic systems are engineered to provide assistance with physical therapy exercises, adapting to individual patient needs and tracking progress. Functionality extends to supporting activities of daily living, promoting independence in tasks such as feeding or grooming. Beyond physical assistance, designs incorporate features aimed at improving quality of life, including social interaction capabilities and cognitive stimulation, all while adhering to safety protocols within a residential care environment.
Sleep disorder clinic robots are designed to gather physiological data during sleep studies, including metrics such as EEG, EMG, EOG, and respiratory effort. These robots facilitate therapy by delivering targeted stimuli – like precisely timed light or sound – and automating repetitive tasks during treatment protocols. Crucially, they incorporate patient feedback mechanisms, allowing individuals to report subjective experiences – such as perceived sleep quality or discomfort – directly into the data stream for analysis, providing a more comprehensive assessment than traditional methods alone.
From Conceptualization to Validation: Iterative Prototyping in Robotic Healthcare Design
Storyboarding in robotic interaction design involves creating a sequence of static images or sketches that depict the intended workflow between a robot, patients, and healthcare staff. This visual method allows designers to map out the steps of an interaction – from initial approach to task completion – and identify potential usability issues or safety concerns before any physical prototyping begins. By illustrating the robot’s actions, the environment, and the anticipated responses of users, storyboarding facilitates early-stage communication among the design team and stakeholders. The resulting storyboards serve as a low-cost, easily-modified tool for iterating on interaction sequences and ensuring that the final robotic system aligns with clinical needs and user expectations.
Cardboard prototyping is a design technique employed to quickly realize and assess robotic concepts using inexpensive and readily available materials. This method prioritizes speed and iterative feedback over aesthetic polish or functional complexity; robotic form factors are approximated with cardboard, tape, and basic components to create a physical representation of the intended design. Healthcare professionals and patients can then interact with this low-fidelity prototype to evaluate usability, identify potential workflow issues, and provide direct feedback on the robot’s size, reach, and overall interaction approach, all before significant investment in more complex and costly development stages. The resulting data informs design refinements and ensures alignment with user needs and practical constraints.
Full-scale prototyping involves the construction of complete, functional robotic systems intended to replicate the final product as closely as possible. These prototypes are not merely aesthetic representations; they incorporate all planned hardware and software components, allowing for comprehensive testing of robot functionality, navigation, manipulation, and human-robot interaction. Evaluation during this stage focuses on identifying and resolving integration issues, validating performance metrics against design specifications, and gathering data on system reliability and safety. Refinement based on full-scale prototype testing informs final design decisions and prepares the robot for clinical trials and eventual deployment.
Iterative prototyping, encompassing stages from storyboarding to full-scale robot construction, is crucial for developing healthcare robotics that are user-centered and contextually appropriate. This process allows designers to identify and address usability issues, safety concerns, and environmental constraints early in development. Specifically, each iteration provides opportunities to gather feedback from clinical staff and patients, ensuring the robotic system’s workflows align with existing healthcare procedures and do not introduce unintended operational challenges. By progressing from low-fidelity models to functional prototypes, developers can systematically refine the robot’s interaction design and functionality, ultimately delivering a system optimized for the specific requirements of its intended healthcare environment and user base.

Specialized Robotic Roles: Defining Functionality for Optimized Healthcare Delivery
The Emergency Department Robot Design envisions a streamlined workflow through dedicated robotic roles. A Patient Registration Robot automates the initial check-in process, reducing administrative burdens and wait times. Simultaneously, a Waiting Room Robot actively engages patients, providing information, entertainment, and potentially even preliminary symptom assessment. Complementing these patient-facing robots, a Supply Delivery Robot efficiently transports medications, linens, and other essential resources throughout the department, freeing up nurses and technicians to focus on direct patient care. This tiered system aims to optimize resource allocation and improve overall efficiency within the often-chaotic environment of an emergency department.
The design of robots for long-term rehabilitation facilities centers on the ‘Rehabilitation Assistance Robot’, conceived to actively support patients throughout their recovery journey. This robotic system isn’t intended to replace human therapists, but rather to augment their efforts and extend the reach of care beyond scheduled sessions. Prototypes emphasize adaptable assistance, providing guidance during exercises, monitoring patient progress through sensor data, and offering motivational feedback. Crucially, the design prioritizes patient safety and intuitive interaction, featuring compliant actuators and user-friendly interfaces. This approach aims to foster independence, improve adherence to therapy plans, and ultimately enhance functional outcomes for individuals undergoing prolonged rehabilitation.
The design of robotic assistance within sleep disorder clinics centers on two key functionalities: comprehensive data collection and personalized feedback. The ‘Sleep Therapy Support Robot’ continuously monitors patient biometrics during sleep studies – including heart rate variability, respiratory patterns, and movement – providing a richer dataset than traditional polysomnography. This data feeds into an ‘Interactive Feedback System’ which then tailors therapeutic interventions and provides patients with real-time insights into their sleep quality, promoting behavioral changes and adherence to treatment plans. This approach moves beyond generalized therapies, enabling clinicians to create highly individualized care pathways informed by objective, robot-collected data and delivered through an engaging, interactive system.
The evolving landscape of healthcare is increasingly benefiting from targeted robotic solutions, and recent research highlights a successful approach to their development. A series of co-design workshops brought together diverse stakeholders – clinicians, patients, and roboticists – to identify specific challenges within emergency departments, rehabilitation facilities, and sleep disorder clinics. This collaborative effort didn’t simply brainstorm ideas; it yielded detailed prototypes for robots designed to automate patient registration, engage waiting patients, deliver supplies, assist in rehabilitation, and support sleep therapy. Crucially, the workshops also produced actionable guidelines for future robotic healthcare development, demonstrating that a multidisciplinary, co-design process is not only feasible but essential for creating robotics that truly address existing pain points and demonstrably improve patient outcomes.
The progression detailed within this research-from abstract concepts to high-fidelity prototypes-mirrors a pursuit of mathematical elegance in engineering. The 14-week co-design workshop series, with its emphasis on iterative prototyping, isn’t merely about building functional robots; it’s about refining a solution through rigorous, repeated application of design principles, much like proving a theorem. G.H. Hardy observed, “The essence of mathematics lies in its elegance and its ability to reveal the truth.” This pursuit of truth, translated to robotics, necessitates a solution grounded in demonstrable correctness, moving beyond simple functionality to a provably effective design integrated seamlessly into complex healthcare workflows. The focus on longitudinal study and workflow analysis ensures the resultant robots aren’t merely conceived in theory, but validated in practice, a vital step towards achieving a truly elegant and robust system.
The Path Forward
The presented work, while documenting a commendable effort in collaborative design, implicitly highlights the foundational ambiguities inherent in translating abstract ‘needs’ into concrete robotic systems. The fourteen-week workshop, a temporal constraint in itself, skirts the deeper issue: a formal specification of ‘considerate’ behavior remains elusive. Workflow analysis, however meticulous, provides only a descriptive layer; it does not prescribe a provably correct instantiation of empathetic robotic action. The current approach risks perpetuating a cycle of empirical refinement – observing, adjusting, repeating – without ever arriving at a mathematically sound basis for ‘considerate’ interaction.
Future investigations must prioritize the formalization of high-level goals. The notion of a ‘need’ requires decomposition into logically verifiable sub-goals. What constitutes ‘situated’ behavior demands a precise definition of the robot’s perceptual capabilities and the associated state space. Simply iterating through prototypes, however aesthetically pleasing or empirically successful, offers no guarantee of robustness or generalization. The field requires a shift from demonstrating ‘works on test cases’ to proving algorithmic correctness with respect to a formally defined ethical framework.
Ultimately, the challenge lies not in building robots that appear considerate, but in constructing systems whose actions are demonstrably aligned with provably correct definitions of human well-being. Until then, the pursuit of ‘considerate’ embodied AI remains a sophisticated form of applied phenomenology, valuable perhaps, but lacking the rigor expected of a true science.
Original article: https://arxiv.org/pdf/2602.03054.pdf
Contact the author: https://www.linkedin.com/in/avetisyan/
See also:
- Clash of Clans Unleash the Duke Community Event for March 2026: Details, How to Progress, Rewards and more
- eFootball 2026 Jürgen Klopp Manager Guide: Best formations, instructions, and tactics
- MLBB x KOF Encore 2026: List of bingo patterns
- Brawl Stars February 2026 Brawl Talk: 100th Brawler, New Game Modes, Buffies, Trophy System, Skins, and more
- Gold Rate Forecast
- eFootball 2026 Starter Set Gabriel Batistuta pack review
- Magic Chess: Go Go Season 5 introduces new GOGO MOBA and Go Go Plaza modes, a cooking mini-game, synergies, and more
- Overwatch Domina counters
- ‘The Mandalorian and Grogu’ Trailer Finally Shows What the Movie Is Selling — But is Anyone Buying?
- Breaking Down the Ruthless Series Finale of Tell Me Lies
2026-02-04 07:44