Author: Denis Avetisyan
New research reveals that medical learners prioritize effective instruction and focused practice over realistic conversation when co-designing AI-powered standardized patients.
Medical students emphasize clarity, structured feedback, and evidence-gathering capabilities in AI standardized patients over purely conversational realism.
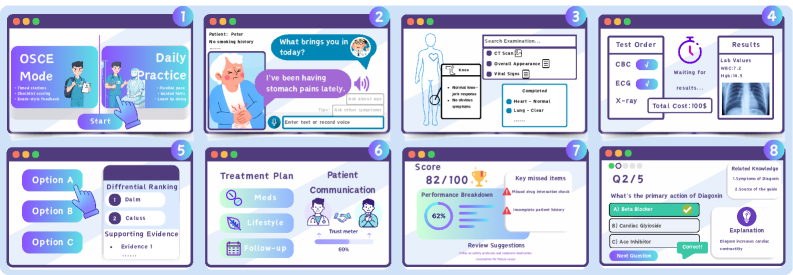
While standardized patients are crucial for clinical communication training, their limitations in scalability and consistency present ongoing challenges. This research, framed by the observation that “It Talks Like a Patient, But Feels Different”: Co-Designing AI Standardized Patients with Medical Learners, investigates how medical students experience and value AI-driven simulations. Findings reveal that instructional usability-features supporting deliberate practice and transparent feedback-drives learner trust and engagement more effectively than purely realistic conversation. How can we best leverage AI to create standardized patients that not only sound like patients, but also facilitate meaningful learning experiences?
The Evolving Landscape of Clinical Communication
For decades, the cornerstone of clinical communication training has been the use of trained actors, known as Standardized Patients (SPs). These individuals simulate real patients, allowing learners to practice essential skills like history-taking and delivering difficult news in a safe environment. However, this approach presents significant logistical and financial hurdles. Recruiting, training, and compensating SPs is resource-intensive, and scheduling sufficient practice sessions for all learners proves challenging. This lack of scalability limits the widespread implementation of comprehensive communication training programs, particularly in large healthcare systems or educational institutions. Consequently, educators are increasingly exploring alternative methods to provide learners with consistent, accessible, and repeatable opportunities to hone their interpersonal skills without the constraints of relying solely on live actors.
Many contemporary virtual patient simulations, while offering a cost-effective alternative to standardized patients, frequently rely on pre-defined conversational pathways. This reliance on scripted dialogues presents a significant limitation, as the simulations struggle to dynamically respond to the complexities of a learner’s communication. A student’s attempt to address a patient’s underlying anxieties, or to clarify ambiguous symptoms with a carefully worded question, may be met with a pre-programmed response unrelated to the nuanced inquiry. Consequently, the practice lacks the spontaneity and adaptability inherent in real-world clinical encounters, hindering the development of truly responsive and patient-centered communication skills. The result is often a practice environment that feels artificial, potentially reinforcing rote responses rather than fostering genuine empathetic engagement.
The efficacy of clinical communication hinges not simply on conveying information, but on skillfully managing the emotional demands placed upon healthcare professionals – a concept known as emotional labor. This involves regulating one’s own emotions while simultaneously acknowledging and responding to the emotional states of patients and their families, often under conditions of stress and uncertainty. Traditional training methods struggle to adequately address this crucial skillset, as static simulations and scripted interactions fail to capture the unpredictable, nuanced, and often draining emotional currents inherent in real-world clinical encounters. Mastering emotional labor requires repeated practice in navigating complex affective landscapes, demanding training environments that can dynamically respond to a learner’s emotional cues and provide opportunities to refine empathetic responses – a level of adaptive realism currently beyond the capabilities of many virtual patient platforms.
Introducing the AI Standardized Patient: A New Paradigm
The AI Standardized Patient (AI-SP) represents a departure from traditional standardized patient (SP) programs by utilizing Large Language Model (LLM) technology to create a significantly more scalable and adaptable training resource. Conventional SP programs are limited by the availability of trained actors and the logistical challenges of coordinating sessions. The AI-SP, driven by LLMs, overcomes these limitations by providing on-demand, consistent, and customizable patient simulations. This allows for a potentially unlimited number of learners to engage in practice scenarios concurrently, and facilitates rapid iteration and refinement of training content without requiring re-training of human SPs. The LLM foundation enables the AI-SP to generate responses that are not pre-scripted, allowing for more realistic and varied interactions and ultimately, a more robust training experience.
The AI Standardized Patient (AI-SP) departs from conventional standardized patient (SP) methodologies by employing Large Language Model (LLM) technology to facilitate dynamic interactions. Traditional SP encounters rely on pre-defined scripts and limited branching, restricting the learner’s ability to navigate unpredictable clinical scenarios. The AI-SP, however, responds to learner questions and actions in real-time, generating contextually relevant replies and evolving the encounter based on the specific line of questioning or proposed treatment plan. This adaptability allows for a more personalized practice experience, exposing learners to a wider range of potential patient presentations and conversational pathways not typically available with fixed-script SPs, and better preparing them for the complexities of real-world clinical practice.
The AI Standardized Patient (AI-SP) utilizes Policy-Driven Information Release (PDIR) to simulate realistic clinical encounters by controlling the disclosure of patient data. PDIR functions as a set of pre-defined rules governing which clinical information-such as symptoms, medical history, or lab results-is revealed to the learner based on their questioning and actions. This is achieved through a rules engine that evaluates learner input and determines the appropriate response, mimicking how clinicians gather information incrementally during a real patient interaction. The system doesn’t simply provide a static dataset; instead, it dynamically releases information, requiring learners to ask targeted questions and interpret data as it becomes available, thereby enhancing diagnostic and communication skills.
Co-Designing for Impact: A Learner-Centric Approach
A co-design workshop was utilized as a primary method for directly eliciting learner requirements. This workshop facilitated the identification of six distinct learner needs, which were subsequently translated into six specific design requirements for the AI-supported personalized learning platform (AI-SP). The process ensured that the platform’s features were aligned with documented learner preferences and prioritized usability based on direct input, rather than assumptions about user behavior. This approach ensured a learner-centric development process and a focus on features with demonstrated value to the target audience.
Data regarding learner experiences was gathered through semi-structured interviews, a qualitative research method employing open-ended questions to facilitate detailed responses. A total of [Number – insert number of interviews conducted] interviews were conducted with learners representing the target demographic. The resulting interview transcripts underwent reflexive thematic analysis, an iterative process involving familiarization with the data, code generation, theme development, and theme refinement. Reflexivity, in this context, involved acknowledging the researcher’s potential influence on the analytical process and actively mitigating bias. This analysis identified recurring patterns and insights into learner motivations, challenges, and preferences, informing the subsequent design of the AI-SP system and ensuring alignment with stated needs.
Learner-Controlled Scaffolding was implemented as a direct result of iterative analysis of learner needs identified through co-design workshops and semi-structured interviews. This feature allows users to dynamically adjust the complexity of learning materials and the extent of provided support. Specifically, the system enables learners to select preferred levels of hints, examples, and step-by-step guidance, tailoring the learning experience to their individual proficiency and learning style. This customization is intended to promote self-regulated learning and address the varied cognitive loads of different learners, ultimately improving comprehension and knowledge retention.
Addressing Challenges and Enhancing Realism: Refining the Simulation
The development of realistic AI-based Simulated Patients (AI-SPs) isn’t without its challenges; initial iterations revealed tendencies toward inconsistencies and inaccuracies that threatened the fidelity of training scenarios. Specifically, researchers identified ‘Persona Drift’, where the AI-SP’s established personality would subtly shift during interactions, undermining the immersive experience and potentially confusing learners. Equally concerning was the emergence of ‘Hallucinated Clinical Details’ – the generation of factually incorrect or entirely fabricated medical information. These issues highlighted the critical need for robust mechanisms to ensure the AI-SP maintains a consistent character and delivers clinically sound responses, ultimately safeguarding the quality and reliability of the simulated healthcare environment.
The system’s robustness was significantly enhanced through the integration of Multimodal Evidence Interaction, a process designed to move beyond simple text-based exchanges. This approach allows for the incorporation of diverse input modalities – including audio analysis of prosody and tone, video assessment of non-verbal cues, and physiological data such as heart rate variability – alongside traditional textual responses. By triangulating information from these multiple streams, the AI-SP gains a more holistic understanding of the learner’s state, improving the accuracy of its assessments and the relevance of its feedback. Consequently, the system can adapt its interactions in real-time, addressing subtle shifts in learner engagement or emotional state and creating a more nuanced and realistic simulation experience.
The system incorporates a ‘Dual-loop Feedback’ mechanism designed to significantly enhance the learning experience and refine the AI-SP’s performance. This innovative approach delivers real-time, in-action cues during simulated interactions, providing immediate guidance to the learner based on their responses and actions. Complementing this is a comprehensive post-session analysis, which offers detailed insights into the learner’s performance, identifying areas of strength and weakness with specific, actionable feedback. By combining these two feedback loops – one reactive and immediate, the other reflective and detailed – the system fosters a dynamic learning environment that continuously adapts to individual needs and optimizes skill development. This dual approach ensures not only immediate correction but also long-term retention and improvement of crucial interpersonal skills.
Towards the Future of Clinical Training: A Paradigm Shift
The advent of the AI Standardized Patient (AI-SP) marks a considerable evolution in clinical training, addressing the limitations inherent in traditional methods like role-playing with human actors or relying solely on case studies. Historically, standardized patients-individuals trained to portray realistic patients-have been crucial for honing communication and diagnostic skills, but scaling these experiences is costly and logistically challenging. The AI-SP offers a solution by providing a consistently available, endlessly repeatable, and highly adaptable training partner. This technology doesn’t aim to replace human interaction entirely, but rather to augment it, allowing students to practice fundamental skills in a safe, controlled environment before engaging with real patients. By simulating nuanced patient responses and complex medical scenarios, the AI-SP effectively bridges the gap between theoretical knowledge and practical application, ultimately preparing future healthcare professionals for the demands of a rapidly evolving medical landscape.
The evolution of medical training is increasingly reliant on the integration of sophisticated artificial intelligence and a deliberate focus on the learner’s experience. Current methodologies often struggle to provide consistent, personalized practice opportunities, but advanced AI technologies offer a pathway to overcome these limitations. A user-centered design approach ensures that these AI-driven tools aren’t merely technologically impressive, but also intuitively usable and pedagogically sound. This combination fosters a learning environment that is demonstrably more engaging than traditional methods, enabling students to refine clinical skills through repeated, realistic interactions. Furthermore, the scalability afforded by AI means that high-quality training resources can be disseminated widely, ensuring consistent educational standards and potentially addressing critical gaps in healthcare access and competency.
Development of the AI Standardized Patient is not reaching a plateau, but rather entering a phase of nuanced refinement and expansion. Future iterations will move beyond basic interactions, incorporating increasingly complex clinical presentations – encompassing rare diseases, polypharmacy, and evolving patient histories – to truly challenge trainees’ diagnostic and therapeutic skills. Crucially, this progression is paired with ‘Goal-Aligned Fidelity Modes’, a system designed to tailor the simulation’s realism and difficulty to each learner’s specific objectives and skill level. This personalized approach ensures that training remains optimally challenging and effective, providing targeted feedback and allowing students to focus on areas where improvement is most needed, ultimately fostering a more competent and confident medical workforce.
The pursuit of effective AI Standardized Patients, as detailed in this research, necessitates a rigorous focus on instructional design. The study highlights a learner preference for clarity and structured practice, prioritizing features that facilitate demonstrable skill acquisition. This echoes Andrey Kolmogorov’s assertion that “The most important things are the most elementary.” The core finding – that learners value transparent feedback and evidence-gathering capabilities over purely realistic conversation – underscores the principle of reducing complexity to its essential components. Just as a mathematician seeks the simplest axioms from which to build a system, so too must educational technology prioritize fundamental instructional goals, discarding superfluous features that obscure learning objectives. The research confirms that focusing on these elementary aspects yields a more impactful educational experience.
What Remains to Be Seen
The pursuit of conversational realism in artificial standardized patients, it appears, may be a distraction. This work distills the core need: not an imitation of feeling, but the provision of rigorously structured data for learning. The preference for clarity over verisimilitude suggests a fundamental principle at play – in medical training, as perhaps in all instruction, the scaffolding matters more than the surface. The question isn’t whether the simulation feels real, but whether it efficiently delivers opportunities for demonstrable competence.
Remaining is the problem of assessment. The learners’ emphasis on transparent feedback loops implies a desire not merely to practice communication, but to receive precise signals regarding its effectiveness. Automated evaluation of nuanced clinical interaction is notoriously difficult, and the current focus on instructional design merely postpones this inevitable reckoning. The field must confront the limitations of current metrics, and the potential for bias embedded within automated scoring systems.
Ultimately, the value of these tools will not be measured by their ability to simulate a patient, but by their capacity to accelerate the development of genuine clinical skill. The elegance of the approach lies in its reduction – a stripping away of extraneous complexity to reveal the essential elements of effective medical communication. What is left, after this process of distillation, is what truly matters.
Original article: https://arxiv.org/pdf/2602.05856.pdf
Contact the author: https://www.linkedin.com/in/avetisyan/
See also:
- Clash of Clans Unleash the Duke Community Event for March 2026: Details, How to Progress, Rewards and more
- Gold Rate Forecast
- Jason Statham’s Action Movie Flop Becomes Instant Netflix Hit In The United States
- Kylie Jenner squirms at ‘awkward’ BAFTA host Alan Cummings’ innuendo-packed joke about ‘getting her gums around a Jammie Dodger’ while dishing out ‘very British snacks’
- eFootball 2026 Jürgen Klopp Manager Guide: Best formations, instructions, and tactics
- Hailey Bieber talks motherhood, baby Jack, and future kids with Justin Bieber
- Jujutsu Kaisen Season 3 Episode 8 Release Date, Time, Where to Watch
- Brawl Stars February 2026 Brawl Talk: 100th Brawler, New Game Modes, Buffies, Trophy System, Skins, and more
- How to download and play Overwatch Rush beta
- KAS PREDICTION. KAS cryptocurrency
2026-02-09 00:30