Author: Denis Avetisyan
A new socially assistive robot, Mobirobot, is being co-developed with clinicians to enhance mobilization exercises for children undergoing rehabilitation and psychiatric treatment.

This paper details the interprofessional and agile development process of Mobirobot, alongside its initial clinical deployment and integration into therapeutic settings.
While robotic assistance holds considerable promise for paediatric rehabilitation, successful clinical integration demands more than technical functionality. This paper details the interprofessional and agile development of Mobirobot – a socially assistive robot designed to facilitate mobilization exercises for children recovering from trauma, fractures, or experiencing psychiatric challenges. Through a co-development process involving clinicians and end-users, Mobirobot achieves adaptable exercise routines and motivational dialogue within dynamic inpatient settings. Can this stakeholder-led approach pave the way for wider adoption of socially assistive robotics in paediatric healthcare and beyond?
Addressing the Limitations of Pediatric Rehabilitation
Pediatric rehabilitation frequently encounters obstacles in delivering sustained, motivating therapy, largely due to practical limitations in therapist access. Children recovering from injury or illness require frequent, consistent intervention to rebuild strength, mobility, and function, yet healthcare systems often struggle to meet this demand. This scarcity of readily available therapists can lead to gaps in care, potentially hindering a child’s progress and prolonging recovery timelines. Consequently, innovative solutions are needed to extend the reach of therapeutic interventions, providing continuous support even when direct, one-on-one sessions are not feasible, and ensuring that young patients receive the consistent engagement necessary for optimal outcomes.
Pediatric patients recovering from abdominal trauma or fractures often present unique rehabilitation challenges demanding highly adaptable and intensive physiotherapy programs. Unlike adult recovery, children require interventions tailored to their developmental stage and fluctuating pain levels, necessitating frequent adjustments to treatment plans. Successful inpatient care hinges on bridging the hospital stay with a robust outpatient strategy, ensuring continuity of exercise and functional skill development. This integrated approach is particularly crucial for maintaining progress and preventing secondary complications like muscle atrophy or contractures, which can significantly impede a child’s return to pre-injury activity levels. Consequently, specialized programs emphasizing early mobilization, pain management, and family education are essential components of comprehensive care, allowing for a more effective and sustained recovery trajectory.
Pediatric rehabilitation frequently encounters complexities when addressing co-occurring mental health conditions, such as depression and anxiety, which can significantly impede physical recovery. These psychological factors often exacerbate functional limitations and diminish a child’s motivation to participate in therapy, creating a cyclical challenge. Traditional rehabilitation protocols, while effective for physical impairments, may not adequately integrate strategies to manage these emotional barriers. Consequently, a growing body of evidence supports the implementation of holistic approaches – integrating mental health support, such as cognitive behavioral therapy or mindfulness techniques – alongside conventional physiotherapy. Such integrated care aims to address the interplay between physical and emotional well-being, fostering resilience, improving treatment adherence, and ultimately optimizing functional outcomes for young patients navigating both physical and psychological challenges.
The future of pediatric rehabilitation increasingly relies on the development of novel therapeutic tools designed to enhance traditional care pathways. These innovations aren’t intended to replace therapists, but rather to extend their reach and personalize treatment plans for each young patient. Such tools could range from gamified exercises that make physiotherapy more engaging – effectively turning recovery into a fun challenge – to virtual reality environments that simulate real-world scenarios for targeted skill practice. Crucially, these advancements also allow for data-driven insights, enabling therapists to monitor progress with greater precision and adjust interventions accordingly. By fostering intrinsic motivation and providing adaptable, intensive support, these tools promise to empower young patients and optimize their recovery journey, particularly for those facing complex conditions or requiring long-term rehabilitation.
Introducing the Mobirobot: A Socially Assistive Intervention
The Mobirobot is a Socially Assistive Robot (SAR) engineered to facilitate the mobilization of pediatric patients – specifically children and adolescents – within both physiotherapy and psychiatric treatment contexts. This targeted application distinguishes it from general-purpose robotics; its design prioritizes interventions aimed at improving motor function and encouraging engagement in therapeutic exercises for physical rehabilitation, as well as providing support and encouragement during psychosocial interventions. The system is intended for use as a clinical tool, working alongside therapists to enhance patient outcomes in these specialized healthcare areas.
The Mobirobot utilizes the NAO robot platform and incorporates pose recognition technology to monitor patient movements during therapeutic exercises. This capability involves the use of visual sensors and algorithms to identify and track specific body positions and ranges of motion. The system then provides immediate auditory or visual feedback to the patient, guiding them through correct form and assisting with exercise completion. Data collected from pose recognition is also available to clinicians for monitoring patient progress and adjusting treatment plans. The NAO platform’s onboard processing capabilities allow for real-time analysis and feedback without external computational requirements.
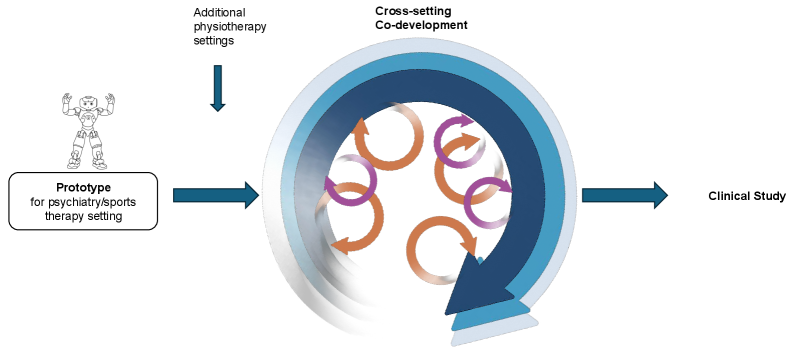
The Mobirobot’s development prioritizes a Co-Development Process, which involves iterative refinement of the system through continuous collaboration with clinicians and patients. This approach is fundamentally guided by Human-Centered Design principles, ensuring that the robot’s functionalities and interaction methods are directly informed by the needs and preferences of end-users. Data gathered from clinical settings and patient feedback loops are incorporated throughout the development lifecycle, driving adjustments to both hardware and software. This cyclical process of design, implementation, evaluation, and refinement aims to maximize the usability, effectiveness, and acceptance of the Mobirobot within therapeutic interventions.
The Mobirobot’s development prioritizes iterative refinement through a co-development process involving clinicians and patients. This methodology utilizes agile software development principles, enabling rapid prototyping and adaptation based on user feedback gathered throughout testing phases. Consequently, the system’s features and functionality are directly informed by the practical requirements of clinical settings, facilitating its integration into existing workflows with minimal disruption. This collaborative approach extends beyond initial development, with provisions for ongoing updates and customization to address evolving clinical needs and ensure long-term usability.
Evidence of Personalized Exercise and Motivational Feedback
The Mobirobot system provides a pre-programmed exercise program intended to facilitate recovery across multiple therapeutic contexts. These include inpatient physiotherapy (InST), inpatient sports therapy (InPT), and outpatient physiotherapy and sports therapy (OutPT). The exercise routines are not generic; they have been specifically designed and analyzed for suitability and exclusion criteria within each of these three distinct deployment settings. Currently, the system encompasses a library of 36 categorized exercises, curated to address a range of rehabilitation needs while remaining appropriate for the specific demands and limitations of each therapeutic environment.
The Mobirobot system incorporates motivational feedback mechanisms designed to bolster patient compliance and effort during exercise routines. This feedback isn’t limited to simple encouragement; the system aims to actively influence patient behavior by providing cues correlated with performance and progress. The intent is to reduce patient discouragement, maintain engagement with the rehabilitation program, and ultimately improve adherence to prescribed exercise plans, thereby maximizing therapeutic outcomes. This is achieved through real-time responses and potentially personalized messaging tailored to individual patient needs and performance metrics.
Mobirobot utilizes pose recognition technology to continuously monitor patient form and performance during exercise routines. This real-time assessment allows the system to dynamically adjust exercise difficulty; if a patient consistently performs an exercise with correct form and minimal effort, the system can increase resistance or complexity. Conversely, if the system detects improper form or struggles with an exercise, it will automatically simplify the movement or provide additional guidance. This adaptive capability is further supported by personalized encouragement delivered based on detected performance levels, aiming to maintain patient motivation and adherence to the prescribed rehabilitation program.
The Mobirobot system utilizes adaptive exercise routines to enhance patient rehabilitation. Currently, the system features a library of 36 categorized exercises, each specifically designed and analyzed for appropriate use in three distinct therapeutic settings: Inpatient Stroke Therapy (InST), Inpatient Physical Therapy (InPT), and Outpatient Physical Therapy (OutPT). This adaptive functionality, driven by performance assessment, aims to increase patient engagement and adherence to their exercise plans, simultaneously reducing the required level of direct therapist supervision and potentially improving overall rehabilitation outcomes.
Sustaining Impact Through Remote Support and Adaptability
The Mobirobot is engineered not just for initial functionality, but for sustained performance through a robust suite of remote servicing capabilities. This proactive approach minimizes disruptions to therapy by enabling rapid diagnosis and resolution of technical issues, often without requiring on-site intervention. Utilizing secure, over-the-air updates and remote diagnostic tools, the system allows for continuous improvement and adaptation to evolving clinical needs. This emphasis on accessibility and efficient maintenance significantly reduces downtime and associated costs, ensuring that the therapeutic benefits of the Mobirobot remain consistently available to patients and clinicians alike, effectively extending the system’s lifespan and maximizing its return on investment.
The Mobirobot leverages advancements in Natural Language Processing to foster a more engaging and effective rehabilitation experience. This technology moves beyond simple command-and-response interactions, enabling the robot to understand and respond to nuanced language from both patients and therapists. By interpreting conversational cues, the system can dynamically adjust therapy exercises, provide encouragement tailored to the patient’s emotional state, and facilitate a more natural dialogue during sessions. This intuitive communication not only enhances patient motivation and adherence but also streamlines the therapeutic process, allowing therapists to focus on individualized care rather than technical operation of the device. Ultimately, this conversational ability positions the Mobirobot as a truly collaborative partner in pediatric rehabilitation, promoting a stronger therapeutic alliance and improved outcomes.
The Mobirobot system is engineered not simply as a therapeutic tool, but as a scalable solution for pediatric rehabilitation. Consistent and accessible remote support is central to this design, allowing the system to be deployed and maintained effectively across diverse clinical environments – from large hospitals to smaller, community-based clinics, and even directly within patients’ homes. This widespread adaptability ensures that a greater number of children can benefit from the Mobirobot’s interventions, regardless of geographical location or access to specialized care. Furthermore, the ability to remotely monitor performance, diagnose issues, and deliver software updates minimizes disruptions and maximizes uptime, enabling a sustained positive impact on a rapidly expanding patient population and fostering a broader reach for innovative rehabilitation techniques.
The Mobirobot isn’t simply a device delivered and left to function independently; its enduring value stems from a commitment to continuous support paired with a fundamentally flexible design. This combination transforms the system from a capital expenditure into a sustained resource for pediatric rehabilitation facilities. Regular remote servicing minimizes disruptions and swiftly addresses technical challenges, ensuring consistent therapeutic access for patients. Crucially, the adaptable design allows the Mobirobot to integrate seamlessly into evolving clinical protocols and accommodate the changing needs of diverse patient populations, effectively future-proofing the investment and maximizing its long-term impact on a child’s recovery journey.
“`html
The development of Mobirobot, as detailed in the article, underscores the importance of deterministic outcomes in complex systems. A robot intended for paediatric rehabilitation demands predictable and reproducible performance; any ambiguity in its actions could compromise therapeutic efficacy and potentially harm a patient. This aligns with Linus Torvalds’ assertion: “Most programmers think that if their code ‘works’ then it’s good. I think that’s a load of baloney.” The co-development approach described, involving iterative testing and refinement with clinicians, directly addresses this need for provable correctness, ensuring that Mobirobot’s movements and interactions are not merely functional, but reliably beneficial and safe for its young patients.
What Remains Constant?
The presented work, while a practical demonstration of robotic assistance in paediatric therapy, merely scratches the surface of a far deeper question. Let N approach infinity – what remains invariant? The immediate challenge is not simply to increase the number of exercises, or even the fidelity of emotional response. It is the formalization of therapeutic intent. Current approaches rely heavily on clinicians defining what constitutes ‘good’ movement, a subjective metric at best. A truly robust system demands a provable link between robotic action and quantifiable physiological improvement, independent of observer bias.
The co-development paradigm, though laudable, introduces its own complexities. The very act of translation – from clinical need to engineering specification – introduces potential for loss of fidelity. The fundamental problem isn’t collaboration, but representation. How does one encode the nuanced understanding of a skilled therapist into a system of algorithms? Current metrics – completion rates, range of motion – are insufficient. They measure what happened, not why it happened, nor whether it truly benefited the patient’s long-term development.
Future work must therefore shift from empirical validation – demonstrating that the robot ‘works’ on a given cohort – to formal verification. Can one prove that the robot’s interventions are, in principle, beneficial? Until that question is addressed, the field risks building increasingly sophisticated tools grounded in intuition, rather than mathematical certainty. The elegance, after all, resides not in the complexity of the mechanism, but in the simplicity of the underlying principle.
Original article: https://arxiv.org/pdf/2601.09838.pdf
Contact the author: https://www.linkedin.com/in/avetisyan/
See also:
- Clash Royale Best Boss Bandit Champion decks
- Vampire’s Fall 2 redeem codes and how to use them (June 2025)
- World Eternal Online promo codes and how to use them (September 2025)
- How to find the Roaming Oak Tree in Heartopia
- Best Arena 9 Decks in Clast Royale
- Mobile Legends January 2026 Leaks: Upcoming new skins, heroes, events and more
- ATHENA: Blood Twins Hero Tier List
- Brawl Stars December 2025 Brawl Talk: Two New Brawlers, Buffie, Vault, New Skins, Game Modes, and more
- Clash Royale Furnace Evolution best decks guide
- How To Watch Tell Me Lies Season 3 Online And Stream The Hit Hulu Drama From Anywhere
2026-01-16 12:25